January 2026 • Thyroid Disorder Clinical Trial Awareness
Thyroid disorder clinical trials play an important role in improving diagnosis, treatment, and long-term management of thyroid conditions that are often overlooked, misdiagnosed, or discovered only after symptoms begin to interfere with daily life.
Thyroid disorders affect millions of people, yet they are frequently underdiagnosed or identified late. Conditions such as hypothyroidism, hyperthyroidism, and thyroid nodules can quietly disrupt metabolism, heart health, mood, fertility, and overall quality of life.
In the United States alone, an estimated 20 million people live with some form of thyroid disease, and nearly 60% remain undiagnosed. Women are significantly more likely to develop thyroid disorders, particularly during periods of hormonal change such as pregnancy or menopause. Despite how common these conditions are, many individuals struggle to find clear answers or personalized treatment options.
That is why thyroid disorder clinical trials are so important. Advances in diagnosis, monitoring, and long-term thyroid treatment all begin with carefully designed research studies. Each clinical trial contributes to a better understanding of how thyroid conditions progress and how care can be improved for future patients.
January is Thyroid Awareness Month, a time dedicated to education, early detection, and highlighting ongoing thyroid research. In that spirit, we are spotlighting five actively recruiting thyroid disorder clinical trials that are exploring new approaches to diagnosis, monitoring, and patient-centered care.
1.Tracking How Thyroid Disorders Develop Over Time
Advancing Diagnostic Precision in Thyroid Disorders
What It’s Studying and Why It Matters
This long-running clinical study focuses on improving how thyroid disorders are identified and classified. Researchers are evaluating advanced diagnostic methods to better understand variations in thyroid hormone function and how they relate to symptoms experienced by patients.
By collecting detailed clinical data and laboratory measurements, the study aims to refine diagnostic pathways that may help reduce delayed or missed diagnoses, one of the biggest challenges in thyroid care today.
Why It Stands Out
Many people with thyroid disease experience symptoms for years before receiving a diagnosis. This study addresses that gap by focusing on diagnostic accuracy rather than treatment alone, which is critical for earlier intervention.
What It Could Mean for Participants
If successful, this research could:
- Improve early detection of thyroid dysfunction
- Support more individualized thyroid treatment plans
- Reduce unnecessary testing and diagnostic uncertainty
Locations
This study is currently recruiting participants at 1 research location in the United States.
Learn more about the study and check your eligibility here.
2. Comparing Two Common Thyroid Medications for Underactive Thyroid
Long-Term Hormone Monitoring in Hypothyroidism
What It’s Studying and Why It Matters
This study is examining how continuous and structured hormone monitoring can improve long-term outcomes for people living with hypothyroidism. Rather than relying on occasional lab tests, researchers are evaluating patterns in thyroid hormone levels over time.
The goal is to better understand why some patients continue to experience symptoms even when lab values appear “normal.”
Why It Stands Out
Hypothyroidism management often follows a one-size-fits-all approach. This trial recognizes that thyroid hormone needs can vary widely between individuals and over time.
What It Could Mean for Participants
This research may:
- Improve symptom management
- Reduce trial-and-error medication adjustments
- Help clinicians tailor thyroid treatment more precisely
Locations
This study is currently recruiting participants at 139 research locations across the United States.
Learn more about the study and check your eligibility here.
3. Reducing Inflammation Before Thyroid Surgery
Non-Invasive Management of Thyroid Nodules
What It’s Studying and Why It Matters
Thyroid nodules are common, especially as people age. This study is exploring imaging-based monitoring strategies that may reduce the need for invasive procedures in individuals with benign thyroid nodules.
Researchers are assessing whether advanced imaging and follow-up protocols can safely replace immediate biopsy or surgery in select patients.
Why It Stands Out
Many thyroid nodules never become clinically significant, yet they often lead to anxiety and unnecessary interventions. This trial focuses on safer, more conservative management.
What It Could Mean for Participants
Potential benefits include:
- Fewer invasive procedures
- Reduced anxiety around nodule monitoring
- Improved quality of life
Locations
This study is currently recruiting participants at 3 research locations in the United States.
Learn more about the study and check your eligibility here.
4. Helping People Decide How to Manage Thyroid Nodules
Improving Early Screening for Thyroid Dysfunction
What It’s Studying and Why It Matters
This early-phase study is testing new screening tools designed to identify thyroid disorders before symptoms become disruptive. The research focuses on individuals who may be at higher risk due to family history or clinical indicators.
Early identification is one of the most effective ways to prevent long-term complications associated with thyroid disease.
Why It Stands Out
There is currently no universal screening approach for thyroid disorders. This study aims to change that by validating tools that could be used more broadly in clinical practice.
What It Could Mean for Participants
If successful, this research could:
- Support earlier diagnosis
- Reduce long-term complications
- Encourage proactive thyroid health management
Locations
This study is currently recruiting participants at 1 research location in the United States.
Learn more about the study and check your eligibility here.
5. A Minimally Invasive Treatment for Non-Cancerous Thyroid Nodules
Understanding Patient Experiences in Chronic Thyroid Disorders
What It’s Studying and Why It Matters
This observational study focuses on patient-reported outcomes, capturing how individuals with chronic thyroid conditions experience symptoms, treatment effects, and daily life challenges.
By prioritizing the patient voice, researchers hope to identify gaps between clinical measurements and real-world experiences.
Why It Stands Out
Thyroid disorders are often managed based on lab results alone. This study emphasizes the importance of listening to patients and incorporating their experiences into future thyroid research.
What It Could Mean for Participants
Findings may:
- Improve patient-centered care
- Influence future trial design
- Help clinicians better address persistent symptoms
Locations
This study is currently recruiting participants at 1 research location in the United States.
Learn more about the study and check your eligibility here.
Moving Thyroid Research Forward
Progress in thyroid care is possible because of individuals who choose to participate in clinical research. Each study contributes valuable insights that help improve diagnosis, monitoring, and long-term management of thyroid disorders.
For those interested in learning more about thyroid disease research and education, trusted resources include the Endocrine Society and ongoing initiatives supported by the National Institutes of Health.
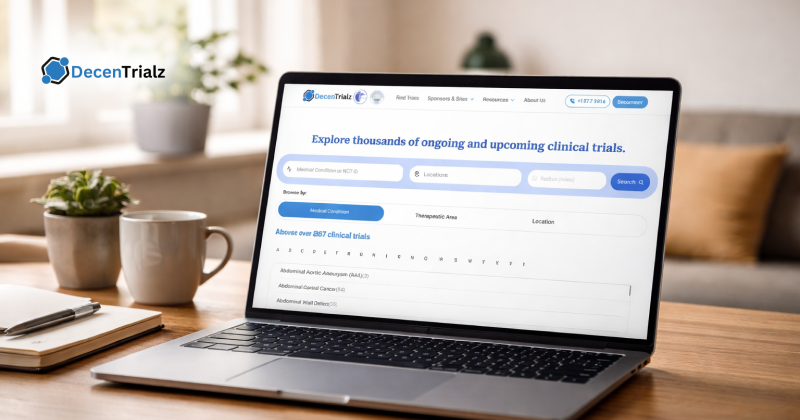
If you are exploring participation opportunities, platforms like DecenTrialz help individuals discover thyroid disorder clinical trials through clear eligibility screening and easy-to-understand study information.